Abstract

Introduction
Minimal residual disease (MRD) negativity after chemoimmunotherapy (CIT) is accepted by the European Medicine Agency as a surrogate parameter for progression free survival (PFS) in CLL. While bone marrow (BM) MRD negativity has been demonstrated to predict response duration even more reliably than MRD negativity in peripheral blood (PB), the prognostic value of immunohistochemistry (IHC) in the BM has not been evaluated. Within the CLL10 trial of the GCLLSG assessing frontline fludarabine, cyclophosphamide, and rituximab (FCR) versus (vs) bendamustine and rituximab (BR), BM MRD by flow cytometry vs IHC was assessed by central laboratories. The prognostic significance of both methods was analyzed here.
Methods
MRD was assessed at a central laboratory by four-color flow cytometry with a sensitivity threshold of 10-4 in PB at study entry, at interim staging, and at final staging in all patients. According to IWCLL guidelines, a BM biopsy was performed at final restaging (FR; i.e. 3 months after the beginning of the last treatment cycle) in patients for confirmation of complete responses. Central BM MRD assessments were done in central laboratories for both, aspirates and trephine biopsies. In the statistical analyses, we compared the associations of MRD levels and IHC by above methods on PFS and overall survival (OS).
Results
310 of 561 included patients (pts) underwent BM biopsy at FR (166 FCR, 144 BR). 209 of 310 BM biopsies were sent to the central laboratory for IHC. 120 (57.4%) of these pts received FCR and 89 (42.6%) received BR. Applying the CLL-IPI, 52 (26.7%) of the pts were in low, 79 (40.5%) in intermediate, 64 (32.8%) in high and 0 (0.0%) in very high risk group. Of the 209 centrally evaluated pts, 135 (64.6%) pts had no BM infiltration (0.0%) by IHC and 74 (35.4%) pts had residual (>0.0%) BM infiltration. Five-year PFS for pts without vs with residual infiltration by IHC was 63.9% vs 34.6% (HR 2.974; CI 1.974-4.482; p<0.0001).
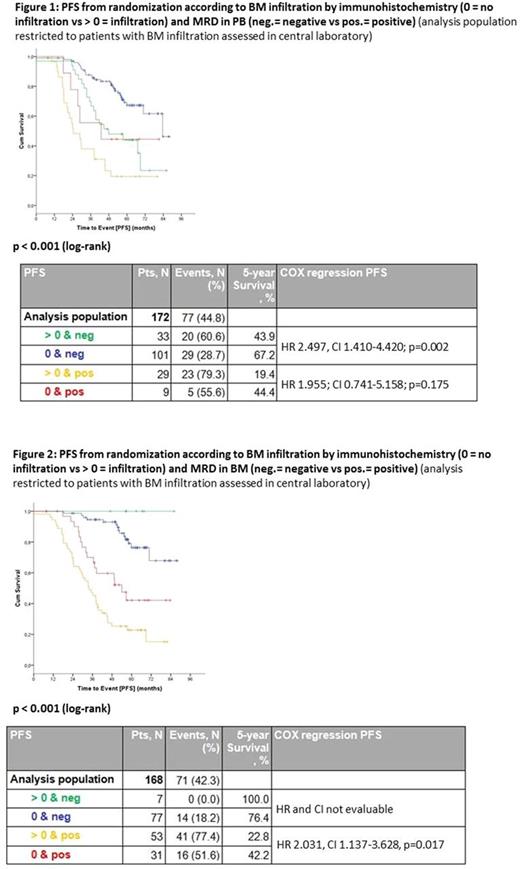
Subsequently, we analyzed PFS according to MRD measured in PB vs BM infiltration. In PB-MRD negative patients PFS at 5 years was 67.2% in the group without residual BM infiltration (N=101) and 43.9 % for pts with infiltration (N=33). PB-MRD positive pts without BM infiltration by IHC (N=9) had a 44.4% 5 year-PFS compared to 19.4% for pts with infiltration (N=29) (Figure 1).
Determining PFS according MRD measured in BM, pts being BM-MRD negative without IHC infiltration (N=77) showed a 5-year PFS of 76.4%, pts with infiltration (N=7) a 100.0% PFS. In contrast, pts with BM-MRD positivity had a 42.2% 5-year PFS when no infiltration by IHC was present (N=31) vs 22.8% for pts with infiltration (N=53) (Figure 2). A discrepancy between BM-IHC and BM-MRD was seen in 7 (4.2%) MRD negative pts with BM infiltration and in 31 (18.5%) MRD positive pts without BM infiltration.
In univariate analyses treatment arm, BM infiltration by IHC, MRD in PB, MRD in BM, del(11q), IGHV mutational status, and serum thymidine kinase levels were identified as prognostic factors for PFS. In multivariate analysis BM-MRD negativity as well as IGHV mutational status remained independent prognostic factors. For OS, no significant differences were observed between pts with or without residual BM infiltration by IHC.
Conclusion
Residual BM infiltration detected by IHC has a significant prognostic impact on PFS after CIT in CLL. However, results from multivariate analyses suggest that BM-MRD negativity measured by flow cytometry has a higher impact on outcome post therapy than IHC. The discrepancies with respect to IHC versus MRD in BM are supposedly methodological. Nevertheless, if flow-based BM MRD analysis is not available, BM IHC might be a helpful parameter to predict post-therapeutic outcome.
Böttcher: Hoffmann La Roche: Honoraria, Other: advisory board, travel support, Research Funding; Mundipharma: Research Funding; Abbvie: Honoraria, Research Funding. Bahlo: F. Hoffmann-LaRoche: Honoraria, Other: travel grants. Kiehl: Roche: Other: Advisory board, travel grants, speakers bureau. Vehling-Kaiser: AbbVie: Consultancy; Lilly: Consultancy; MSD: Consultancy; Amgen: Consultancy; F. Hoffmann-LaRoche: Consultancy; Gilead: Consultancy. Gregor: GlaxoSmithKline: Other: Personal Fees; Gilead: Other: Personal Fees; Celgene: Other: Personal Fees, Non-Financial Support; AbbVie: Other: Personal Fees; Janssen: Other: Personal Fees, Non-Financial Support; Mundipharma: Other: Personal Fees; Novartis: Other: Personal Fees, Non-Financial Support; Roche: Other: Personal Fees, Non-Financial Support. Plesner: Janssen: Research Funding; Janssen, Takeda: Consultancy; Janssen, Genmab: Membership on an entity's Board of Directors or advisory committees. Döhner: Astex Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Honoraria; Celator: Honoraria; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Agios: Honoraria; Sunesis: Honoraria; Seattle Genetics: Honoraria; Pfizer: Research Funding; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol Myers Squibb: Research Funding; Boehringer Ingelheim: Research Funding; Arog Pharmaceuticals: Honoraria, Research Funding; Amgen: Honoraria. Kneba: AbbVie: Consultancy, Honoraria, Other: travel support, Research Funding; F. Hoffmann-LaRoche: Consultancy, Honoraria, Other: travel support, Research Funding; Gilead: Consultancy, Honoraria, Other: travel support, Research Funding; Janssen-Cilag: Consultancy, Honoraria, Other: travel support, Research Funding; Mundipharma: Consultancy, Honoraria, Other: travel support, Research Funding. Wendtner: Abbvie: Other: Personal Fees; Morphosys: Other: Personal Fees; Servier: Other: Grant, Personal Fees; Gilead: Other: Personal Fees; Novartis: Other: Personal Fees; Janssen-Cilag: Other: Personal Fees; Mundipharma: Other: Grant, Personal Fees; Celgene: Consultancy, Research Funding; Hoffmann La Roche: Other: Grant, Personal Fees. Kreuzer: Amgen: Consultancy, Honoraria, Other: Personal Fees, Research Funding; Janssen-Cilag: Consultancy, Honoraria, Research Funding; Gilead: Consultancy, Honoraria, Research Funding; F. Hoffmann-LaRoche: Consultancy, Honoraria, Research Funding; Mundipharma: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding. Stilgenbauer: Mundipharma: Consultancy, Honoraria, Research Funding; Hoffman La-Roche: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Sanofi: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Gilead: Consultancy, Honoraria, Research Funding; Pharmacyclics: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Genzyme: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Genentech: Consultancy, Honoraria, Research Funding; GSK: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Boehringer-Ingelheim: Consultancy, Honoraria, Research Funding. Fink: Hoffmann La Roche: Other: Travel grant; Celgene: Other: Grant; Mindipharma: Other: Travel Grant. Hallek: Roche: Consultancy, Other: Grant, Personal Fees, Research Funding, Speakers Bureau; AbbVie: Consultancy, Research Funding, Speakers Bureau. Klapper: Hoffmann La Roche: Other: Grant; Novartis: Other: Grant; Celgene: Other: Grant; Takeda Millenium: Other: Grant. Eichhorst: Roche: Other: Grant, Personal Fees; Mundipharma: Other: Grant, Personal Fees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal